The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
MAJOR SURGERY PREP
BOWEL PREP INSTRUCTIONS FOR MAJOR SURGERY
Do the day before surgery
It is important for your safety to prepare the colon and small intestines for your operation. Properly prepared
bowels can be operated upon and repaired. Bowels that are not prepared often require a temporary colostomy if
for an unknown reason your bowel is involved with your problem and needs to be included in your operation.
For your protection it is recommended:
The follow- ing instruc-
tions are for the day before surgery!
On the day before surgery drink only clear liquids: beginning at
12:00 noon
A. Gatorade
B. Jell-O
C. Clear broth
D. Coffee or tea (do not add milk or cream)
E. Popsicles
F. Bottled beverage
G. Water
****NO MILK OR MILK PRODUCTS
***NO SOLID FOODS
2. You may take any medication the doctor or nurse tells you to with a small sip of water
3. Drink ½ bottle of Fleets Phosphasoda at 12:00 noon. Drink second ½ at 2:00pm.
Diarrhea will occur shortly thereafter. Some people have experienced rectal/anal burning
during this preparation.
4. Give yourself a fleet enema at 7pm.
5. Do not eat or drink anything after midnight the night before your surgery.
6. On the morning of the operation, medications you are instructed to take should be taken with
a small sip of water.
Buy at the Drugstore:
1. one fleets enema
2. 90 cc of fleets Phosphasoda
Drink 10-15 glasses of liquid dur-
ing the bowel preparation in or-
der to hydrate your body
The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
1. You will need someone with you to drive you home.
2. Do not have anything to eat or drink after midnight on the night before surgery, not even water, juice,
or coffee!
3. Wear comfortable (loose fitting) clothes.
4. Avoid herbs, vitamin E, NSAIDS (Motrin, advil, ibuprofen, naprosyn, Aleve, etc.) and aspirin 1 week
prior to surgery. It will “thin the blood”
5. Take a multivitamin daily.
6. Commit to living a healthy lifestyle. This includes, but is not limited too, Plenty of rest, fresh air,
Sunshine, exercise, good nutrition, positive mental outlook, avoidance of alcohol, tobacco, and
excessive caffeine.
7. These forms are required by the facility at admission, so bring
With you:
a. Pre-operative orders b. Consent Form
c. Post-operative instruction sheet d. Labs
Cancellations of Surgery
Surgery may be cancelled for the following reasons:
1. You choose too.
2. You or your surgeon develop an illness
3. Urinary tract Infection
4. Failure to perform the bowel preparation
5. Some unforeseen emergency or weather phenomenon
6. Failure of your insurance to authorize the surgery
7. Abnormal preoperative clearance (laboratories tests)
8. Failure to keep preoperative appointment

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
Preparing for Surgery
More than 25 million surgical procedures are performed each year in the United States.
This patient education booklet will help you prepare for your surgery. By understanding the different steps, you can
help your healthcare providers ensure a successful operation and a routine recovery.
Our hope is that we will help you to:
• gain a better understanding of your medical condition
• know your treatment options
• understand the risks of surgery - as well as the risk should you decide not to have the treatment
your doctor recommends
• You should also know what to expect on the day of surgery
• and about the recovery process
A planned surgery involves very distinct steps.
Gynecologic evaluation, discussions, and usually a trial of alternative treatments
Decision for surgical treatment
If not already, institution of a healthy living program
Pre-surgical gynecologic office visit/occasionally medical clearance evaluation with your primary care
physician
Hospital pre-surgical visit/visit with anesthesia
Laboratory specimens and other tests as needed
Day of surgery (usually admission day)
Day of Discharge
Postoperative office visit(s)
Release to work (full recovery)
Your Team of Health Care Workers include:
Your Physician and his Surgical Assistant ( in our practice this is a Board Certified Gynecologic Surgeon)
Your Physician’s office staff
Your Primary Care Physician
Hospital Nurses, surgical schedulers, and ancillary help
Anesthesiologist and his/her assistant
Pathologist and laboratory ancillary help
Your insurance Carrier
In today’s complex medical environment, choosing a surgical option for your condition requires guidance, knowl-
edge, sensitivity, and expertise. Thank you for the privilege of assisting you in this process.
Very Truly Yours,
R. Wayne Whitted MD, MPH
Paul A. Pietro MD
Office Staff

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
Information for the Woman Having a Major Gynecologic Operation
Hysterectomy, myomectomy, vaginal repairs, Operative LaparoscopyEt. Cetera
Preparation for Surgery
Once the decision has been made Major Surgery, a time for your surgery will be scheduled. This is a com-
plex process based on hospital availability and yours, the doctor’s, and his/her assistant’s schedule. You probably
will be admitted to the hospital on the morning of your surgery. Prior to the date of your surgery, you will have had
a preoperative checkup by your doctor.
At this visit, you should discuss any questions that you have with your doctor. Routine blood and urine
tests will be ordered. An electrocardiogram or chest X-ray also might be ordered. Instructions for a bowel prep will
be given. At the conclusion of this visit you will be given instructions by the clinical secretary, your postoperative
prescriptions, and your postoperative appointment.
You will be asked to sign a legal surgical consent before surgery. Your doctor should discuss the procedure
with you and answer all of your questions before you are asked to sign the consent. You will be asked also to sign a
consent for blood transfusions if there is a possibility that you will need blood during or after the procedure. If you
prefer to use your own blood, you must make arrangements 3 weeks prior to your surgery date. Contact the Com-
munity Blood Center of South Florida (1-800-357-4483) for details after you discuss it with your doctor.
It is normal to have some concern and anxiety before surgery. The important thing is how you deal with
these emotions. Ask any questions you have, so that you will feel as comfortable as possible before you go to sur-
gery. Often, a woman feels better if she understands what is going to happen to her. We can refer you to a counselor
well-versed in pre-surgical anxiety if you would like. Ask us for this referral if you feel it is necessary.
Prior to surgery, you will visit the anesthesiologist, a doctor who specializes in caring for people during
surgery. The anesthesiologist will discuss the plans for anesthesia for your surgery and answer your questions. You
may be asked to sign a consent after you have visited with the anesthesiologist. You probably will be given a general
anesthesia so you will be asleep (a tube is inserted in your throat) during surgery. Sometimes a spinal or epidural
anesthetic is used. Discuss these options with the anesthesiologist.
It is highly recommended to take a tour of the ward where you will be for you inpatient hospital stay. Dur-
ing this tour important information can be obtained about ward routines and expectations.
Procedures just prior to surgery generally include the following:
● You should go to a liquid diet the day before surgery. After midnight, you should not have anything to eat
or drink. This is called NPO, which means nothing by mouth. You should not chew gum or smoke during
this time. You can brush your teeth the morning of your surgery, but only rinse your mouth and do not
swallow any water. Your stomach must be empty when you are given anesthesia.
● When you are admitted for surgery, tell the nurse if you have any allergies or if you are on a special diet or
taking any medications. Your medications may need to be started again following surgery. NOTIFY
YOUR DOCTOR AND HOSPITAL IF YOU ARE ALLERGIC TO LATEX. LATEX IS PRESENT
THROUGHOUT THE OPERATING ROOM AND SPECIAL PROCEDURES ARE IMPLE-
MENTED IF A PATIENT IS ALLERGIC TO LATEX. FAILURE TO DO THIS MAY CAUSE
YOUR SURGERY TO BE CANCELLED.
● Make sure you accomplish the bowel prep appropriately. This will ensure safety for you in case your opera-
tion includes bowel surgery or significant bowel injury risk.
● Every patient who has a surgical procedure needs to have an IV. Your abdomen and pubic area might be
shaved while you are in the operating room and after you are given your anesthetic. A catheter will be
placed in your bladder during your operation.
● If you have glasses, contacts, dentures, or bridgework, you must remove them before you go to the operat-
ing room. Nail polish and eye makeup also need to be removed. Also, no tampax/tampons should be used
prior to surgery.
You will be taken to the operating room about a half hour before your surgery begins. The surgical procedure
will take from 1-3 hours on the average. This depends on the procedures that are done. Your surgeon will go to
the surgical waiting room and speak to whomever you choose after your surgery is finished. It is important that
family members remain available in the surgical waiting room for consultation.

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
The Pre-surgical Visit
The pre-surgical visit is done prior to surgery. During this visit an anesthesia specialist evaluates you and your
medical history to determine the appropriate anesthesia for you. Usually a physical exam is performed and
questions asked regarding your health. Laboratories, Chest X-Ray, Electrocardiogram may be performed to
confirm your health status.
Questions that might be asked of you include:
● What prescription medications are you taking? Are you taking any non-prescription medications?
● Do you have any allergies to drug or food groups? If yes, what are you allergic too?
● Are you allergic to Latex
● Have you had anesthesia before? If so, were you allergic to any anesthetic drugs? Do you know if any
blood relatives of yours have had anesthetic problems?
● Discuss your medical problems you may have: heart, lung, kidney, liver, mitral valve prolapse, diabe-
tes, high blood pressure, psychiatric disorders
● Have you had blood transfusions in the past? If so, for what reason?
● It is important to tell the anesthesia expert about snoring problems, loose teeth or dental work. Fail-
ure to make them aware may hinder the intubation process.
● It is very important to discuss all medications you are taking to include over-the-counter medications
and herbal supplements. These may interact with anesthesia and reduce your ability to clot your
blood.
● You should discuss what medications you should continue to take even on the morning of the opera-
tion.
● You should inform your doctors and hospital personnel caring for you if you drink alcohol on a daily
basis. Some precautions may need to be taken to prevent you from suffering from alcohol withdrawal
after the surgery.
Based on your answers, the anesthesia expert and surgeon will determine the best anesthetic for you. Anesthe-
sia is a combination of medications and possibly gases that are used so that you don’t feel the discomfort of sur-
gery.
There are three general types of anesthesia:
General Anesthesia (given through a mask/intravenous)
Regional Anesthesia (spinal, epidural, nerve blocks)
Local Anesthesia (usually with intravenous sedation)
Discuss these types with your anesthesia expert.
The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676● www.floridaamigos.com
The Day and Night Before Surgery
To avoid complications during and after your surgery, you must limit what you eat and drink. This is done, because
during surgery, it is possible for the food in your stomach to be vomited and inhaled into the lungs. Do Not eat,
drink, chew, or suck on any food after midnight before your surgery. This includes gum, mints, and candy.
If you are a diabetic ask your doctor when you should eat last.
At your anesthesia visit, you will be told which medications you should take the morning of surgery. They can be
swallowed with a few sips of water right when you wake.
If you are a smoker, it is best for you to stop smoking at least 3 days before surgery. If you cannot stop, you should
at least cut down how much you smoke and stop smoking after midnight the night before surgery. Do not drink
alcoholic beverages within 48 hours of surgery.
The bowel prep is done the day before surgery. Follow closely the instructions given to you by your doctor.
The Day of Surgery
On the day of surgery, you will be admitted to the surgical area and an identity bracelet will be placed around you
wrist. It is best to leave jewelry and other valuables at home. All facial makeup, nail polish, and body piercings
should be removed prior to coming to the hospital.
It is best to wear simple loose-fitting clothes that will not place pressure on the operative site.
You will visit with your surgeon, the anesthesia expert, and your holding-area nurse prior to going to the operating
room. Your medical history will be reviewed. It is important to bring up any issues that have occurred that your
health care providers might not be aware. These may be the recent development of a “cold”, “fever”, urinary tract
infection, etc.
Your surgeon will mark the operative site if it is on one side of your body. It is important to remember what body
part needs the operation.
To have surgery, you need to sign a consent form. Signing the consent form indicates that you know what the sur-
gery is for, understand what the benefits and risks are, and allow the doctors and other hospital staff to proceed with
the surgery.
Once the consent is signed you will be given a sedative through your IV. You will shortly be going to the operating
room.

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
Recovery at Home
Every woman recovers from a major surgical procedure at her own speed. During the first week or
two, just plan to rest and relax. You will be up and around the house, but don’t expect too much
from yourself.
● Gradually increase your activity as you recover. Limit yourself at first, and avoid heavy lifting and household
activities, such as vacuuming. Your doctor might suggest that you not drive a car for about 2 weeks. You need
to feel that you can move about to be a safe driver, and you should not be taking pain pills that can impair your
response time. You will tire easily; so don’t plan too many activities. Just relax and let your body heal.
● We recommend showering for the first 3 weeks. After that you can take tub baths.
● We recommend a bland diet for the first 7 days. After that gradually add back foods you like.
● To avoid constipation, I recommend fiber, surfak, walking, plenty of fluids; and milk of magnesia every other
day. Avoid laxatives. If this is a problem talk with your doctor.
● Take your pain medicine as you need to. Narcotics can be taken every 3 hours. You can take advil or other
non-steroidal anti-inflammatory medications in between. This generally reduces the amount of narcotic nec-
essary. Occasionally a sleeping aid is necessary at night.
● Do not place anything in your vagina (no douches, tampons, or intercourse) until your doctor has examined
you to see that the stitches have completely healed. You can usually expect to resume intercourse after 8
weeks.
● You probably will be able to return to work in 3-6 weeks depending on the type of surgery, the type of work you
do, and your particular desires. Management at your workplace usually has a leave time designated for your
particular type of surgery. You will need to follow those guidelines. If you start back to work early, we recom-
mend working a ½ day for the first week.
● Remember to go slowly and increase your activities as your body recovers. Each woman experiences recovery
in her own way. It is not unusual to feel moody and irritable at times following surgery. This can be caused by
fatigue and should disappear as you recover and resume your normal activities.
● If you experience any of the following, you should call your doctor:
An increase in vaginal bleeding
Redness, swelling, drainage from your incision, or separation of the edges of the incision
Pain in your legs with swelling
Fever or chills (check your temperature before you call the doctor)
Severe chest pain or shortness of breath
● Once your have fully recovered, you should feel like your normal self. This usually takes about 3 months. You
will be free of the discomfort and/or bleeding that you had before your surgery. You will no longer be able to
become pregnant or have your period. If your ovaries were not removed, they should continue to function as
they did before your surgery. If you have been put on estrogen therapy, the estrogen will be replaced in your
body. The estrogen therapy might need to be adjusted by your doctor as your body adapts to the change.
● If your experience vaginal dryness when having intercourse, a water-soluble lubricant, such as K-Y jelly, Re-
plens, Astroglide is appropriate to use. Do not use Vaseline because it does not wash off with water and might
cause problems. It is not unusual for the vaginal tissue to tighten following hysterectomy. Having sexual in-
tercourse actually helps the tissue to lubricate and stretch again. Most women feel that their sexual relations
are better following hysterectomy.
● If you have any questions about your recovery, talk to your doctor at 305-596-3744.
● Pursue a healthy life-style by making sure that you get regular exercise and eat foods that are good for your
body; include fruits and vegetables, low fat meats (chicken and fish), low-fat dairy products, breads and pasta.
Take good care of yourself. You are worth it!
● Menopausal symptoms (hot flushing, insomnia, mood changes, memory and concentration loss) can occur if
your ovaries are removed. These usually will start 2-3 days after surgery. Discuss this with your doctor at your
first postoperative visit.

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
During Surgery
You will be given a gown to wear. The operating team includes a circulating nurse, a scrub nurse, a nurse anesthetist
monitored by an anesthesiologist or an anesthesiologist, equipment support personnel, and your operating surgeon
and his assistant (in our circumstances the assistant is a qualified gynecologic surgeon with credentialed expertise
in all areas of gynecology surgery). Your team will be with you during your entire surgery.
In cases of general anesthesia you will be given some medication through the IV which will sting a little. This medi-
cine makes you go to sleep. An endotracheal tube will be placed in your throat to your lungs to help you breathe.
Anesthetic gases will be given down this tube. You will be continuously monitored while in the operating room.
Monitors will detect your oxygen levels, blood pressure, pulse, respirations.
After anesthesia is induced and before the surgery is begun, a “time-out” is performed. At this time your identity is
verified and the specific surgery to be performed is confirmed by all present in the room.
When the surgery is over you will be awakened in the operating room and the tube will be pulled out of your throat
only when you are able to breathe on your own. Your team will then transport you to the recovery room.
Intubation for breathing
support
Operating Room and Team

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
POSTOPERATIVE RECOVERY
Following the surgery, you will be in the recovery room until you are awake and ready to be transferred to your
room. If your visitors are in the surgery waiting room, they will be informed when your surgery is finished and you
are admitted to the recovery room. Your family will not be able to visit with you until you are cleared from the recov-
ery room. You will spend, on the average, 1-2 hours in the recovery room. Your family will be notified of your status
and when you will be transferred to your room in the hospital.
Many Major Surgeries are considered outpatient because of their minimally invasive approach. This includes Hys-
terectomies. The benefits of going home include more comfort (your own surroundings) and quieter. In addition,
you are at less risk for hospital acquired infections.
You will be allowed to go home when you meet the following criteria
• Tolerating a diet (a minimum is liquids)
• Voiding (urinating) on your own (in most cases)
• Oral pain medicine satisfactorily takes care of the postoperative discomfort
• You feel you are mentally and physically able
Immediate Postoperative Care (if you do not go home)
When you return to your room after surgery, the nurse will check you vital signs frequently. She will encourage
you to turn from side to side, take deep breaths periodically, and to cough. You should hold a pillow or folded blan-
ket against your abdominal incision for comfort while you cough. You will also be asked to use a breathing device
called an incentive spirometer. You will need to inhale strongly to get the blue ball to 1500. All of these exercises
help keep your lungs clear and minimize the chance of getting pneumonia. You will dangle at the bedside the night
of surgery or begin walking depending on your surgery. When you can walk, you will be asked to walk twice in a
shift (8 hours). You will also be encouraged to get out of bed and sit in a chair. In addition compression stockings
will be used until you are fully mobile. All of these exercises are used to minimize your risk to clots in your legs.
During the evening of your surgery, you will be sleepy and will be encouraged to rest. Medication for pain will
be available to you by IV, with a self-dosing pump, by intramuscular injection and subsequently by oral intake. Usu-
ally you will begin oral pill pain control in the morning after surgery. Pain control is of utmost importance for your
postoperative comfort. At times a lidocaine skin patch will be placed near your incisions to reduce postoperative
skin incision pain. These last normally 12 hours and will be removed at that time.
We recommend taking head phones and a CD player to listen to our specially prepared CD of “healing music”. This
music reduces anxiety, stress, and enhances the immune system. This music should be listened too throughout your
entire recovery (and possibly beyond!)
The Next Day (if you do not go home)
You will have oral liquids as soon as you are able to tolerate it and your diet will be advanced as you tolerate it.
The IV will be discontinued once you tolerate a diet, have received all of your antibiotics, and tolerate oral pain con-
trol with good results. Following surgery your bowels slow down because of anesthesia, handling during your sur-
gery, and medications. You will be encouraged to ambulate (walk) 2 times/nursing shift. This will help reduce the
chance of gas pains after surgery. With laparoscopy, one may experience shoulder pain from the gases used to in-
flate the abdomen so the operation can be performed. This usually resolves within 48 hours.
A small tube (catheter) will be inserted into your bladder to drain your urine. The catheter may be inserted into
the bladder through the urethra (opening from the bladder to the outside of the body) or through a small opening on
your abdomen. This type of catheter is called a suprapubic catheter. The catheter usually is removed the morning
after your surgery and sometimes the evening of surgery (depending on the situation). However, if you have some
repair done on your bladder or the vaginal wall, the catheter will remain in place for a few days until you are able to
urinate well on your own. Occasionally with this type of surgery you will be sent home with a catheter in place. You
will be brought into the office to remove the catheter and check the function of the bladder. If you have had a blad-
der injury during your surgery, the catheter will remain in place for about 2-3 weeks (at the discretion of your doc-
tor). This will help prevent the development of a fistula (an opening from your bladder to your vagina). Do not be
discouraged if you cannot empty your bladder well after bladder surgery. This is not uncommon and some have to
be sent home with their catheter in place. An attempt will be made to remove the catheter weekly until successful.

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
Activities and Hygiene
Your first day following surgery, you will be up in the chair and also walking about your room. If you tolerate
this you will be encouraged to walk in the hallways. This will improve circulation and encourage your bowels to be-
gin to function again.
You will be assisted with a shower on the first day after surgery and by the second day, if you are not already
home, you will be ready for a shower alone. You can wash your hair in the shower when you wish. Once you have
showered dry the incision sites well (“pat dry”). They do not need to be covered. Occasionally a blow dryer is
needed to keep the sites dry.
Your incision might have staples, or it might be closed with a suture that dissolves as the tissue heals and does
not need to be removed. You can wash over your incision with soap and water when you shower. The nurses and/or
doctor will look at your incision while you are in the hospital to see that it is healing well and that there are no signs
of infection. If staples are used your doctor will remove the staples about five to seven days after your surgery. The
doctor might put small pieces of tape, called steri-strips, across your incision. Just remove the strips of tape if they
become loose or if they cause irritation. The area around the incision might be swollen and feel hard, but it will im-
prove as the incision heals. The scar will appear red at first and will fade to a white line during the months following
your surgery. Over the course of healing, the incision will itch and sometimes have a tingly sensation. This is nor-
mal.
You could have some vaginal discharge or bleeding following surgery and need to wear a sanitary pad. If you
have bright red bleeding or blood clots, you should tell your nurse or doctor. The vaginal discharge is usually a dark
bloody color or a pink or tan color. This usually improves once healing occurs at about 8 weeks. A small minipad
will be enough protection when you are at home. The stitches used to sew the top of the vagina dissolve at about 21-
25 days after surgery. At this time you may see a little more bleeding and it is normal.
Preparations for Going Home
You will be in the hospital overnight (maybe longer depending on the type of surgery and your individual recov-
ery). With Laparoscopic surgery (including hysterectomy) some women prefer to be discharged the evening of the
operation (outpatient surgery). This is a decision you and your doctor will make. Usually, if you have had vaginal
reconstruction surgery you will be in the hospital for 2 days. Before you leave the hospital, you must be able to toler-
ate an oral diet, take oral pain control, urinate on your own (unless you have had bladder surgery), have no tempera-
ture above 101 F, and feel you are able to go home. Your particular insurance has specific numbers of days you are
allowed to stay in the hospital. It is recommended you discuss this with your insurance carrier prior to surgery to
clarify this issue.
You will need someone with your for at least one week to assist you at home. You will be given any prescrip-
tions you will need for home usually at the preoperative visit. This will include pain medications and any antibiotics
you may need depending on your personal circumstances. You will also need to have your postoperative office visit
scheduled. Your first postoperative visit will be in 7 days from surgery. Generally it is more convenient to have ac-
complished these preoperatively. You will need someone to take you home from the hospital. We generally recom-
mend bed rest with walking just like in the hospital for 7 full days. In addition, we recommend a bland diet for the
first seven days. This will minimize “gas” problems after surgery. Make sure you write your questions down so that
you can discuss them at your postoperative visit. It is also important to take milk of magnesia periodically after sur-
gery. This will help with constipation. Other things you can do to help with constipation are: minimize narcotics,
drink 10 glasses of liquid/day, surfak (over-the-counter), prunes, fiber (Citrucel). Laparoscopic incision sites may
get small hematomas (bruises). These can be particularly tender and advil/motrin is the best for this. Additionally,
a cold pack can help.
For those who have had bladder repair surgery/incontinence surgery:
1. You may be discharged with a catheter attached to a leg bag.
2. You will be instructed on the care of this.
3. You will be brought into the office at a pre-determined time to have the catheter removed.
4. Once the catheter is removed, you must be able to urinate adequately or else the catheter may need to be
replaced.
5. On the average, after bladder repair surgery, it may take 1-2 weeks for the bladder to begin functioning
properly (due to swelling and edema)
The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
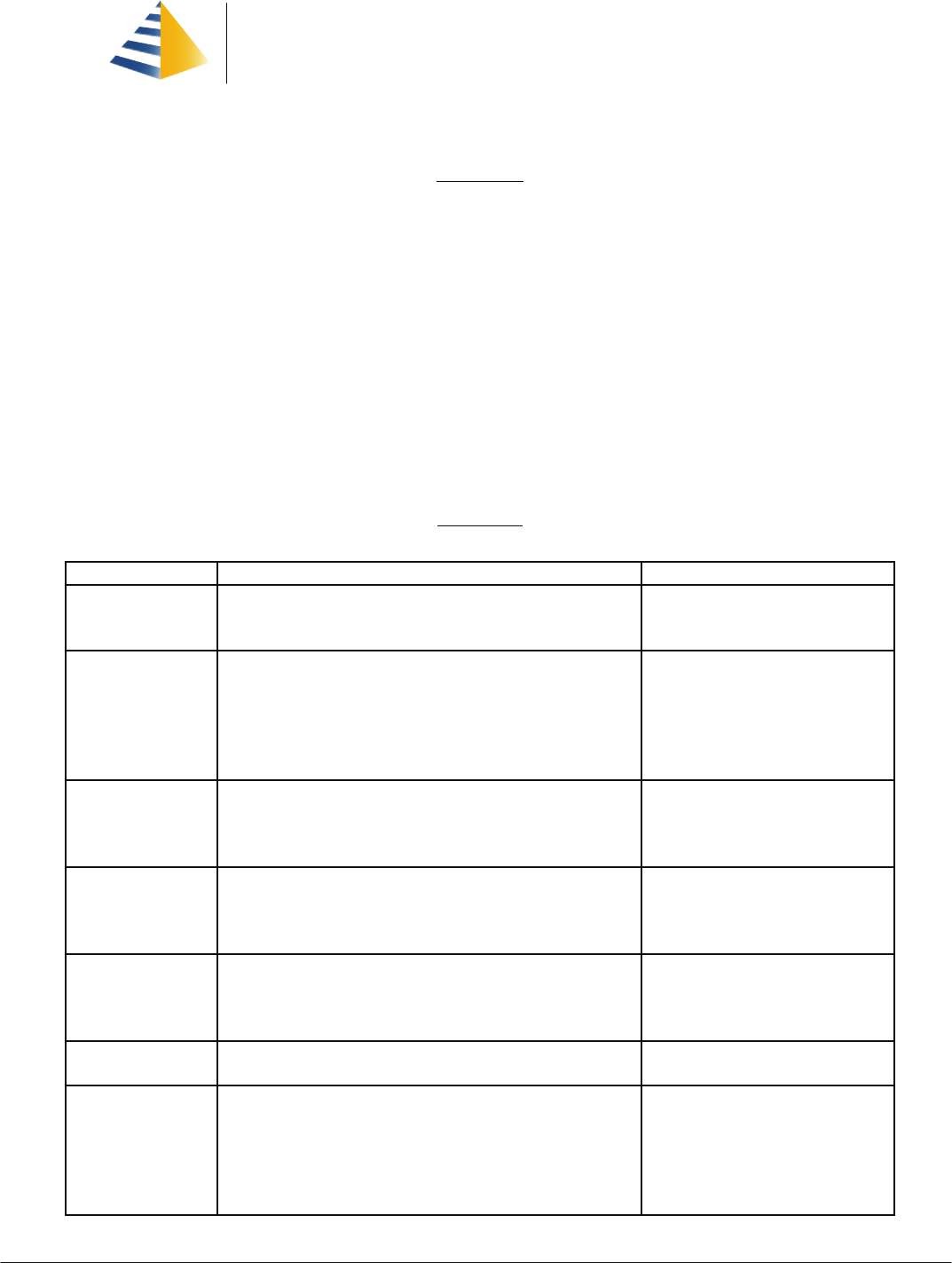
Bland Diet
Purpose:
This diet is designed to provide adequate nutrition during the early postoperative period. It is intended to decrease
irritation of the Gastro-intestinal tract and aid in physical comfort.
Description:
The basic food groups are used for planning nutritionally adequate meals. The diet may vary due to individual food
intolerances and the patient’s lifestyle. Active gastric irritants are avoided. These include caffeine, coffee, decaffein-
ated coffee, tea, cocoa, carbonated beverages containing caffeine, alcohol, chocolate, pepper, chili powder, citrus,
tomatoes, and any other foods that cause individual discomfort. Most foods stimulate gastric secretions and are
therefore not useful as buffers. Three meals per day are recommended, if tolerated, since additional meals stimulate
acid secretion. Avoid bedtime snacks that can stimulate acid production during the night.
Nutritional Adequacy:
The bland diet will meet the requirements for all essential nutrients. We do recommend supplementation with a
well-rounded vitamin (e.g.: Centrum or Centrum silver)
Food Lists
Food Group Foods Allowed Foods to Avoid
Milk and Dairy Whole, low fat or 2%, skim milk,
dry or instant Milk, evaporated milk,
buttermilk, yogurt, cottage cheese, cheese
Chocolate milk or cocoa
Meats and Meat
Substitutes
Lean and tender with visible fat removed; beef, veal, lamb, fresh
pork, cooked medium to well done. Turkey, chicken, Cornish
game hen. Fresh, frozen or canned fish or shellfish. Organ
meats—liver and sweetbreads; eggs
Fried or smoked meats. Processed
ham, sausage, spiced or highly sea-
soned meats such as frankfurters
and luncheon meats. Fried eggs
Potatoes and Substi-
tutes
Plain or buttered white rice, macaroni, noodles, spaghetti; white
potato baked, served without skin, boiled, mashed, diced or
creamed. Sweet potato and yams.
Fried potatoes. Any with seasonings
not allowed
Breads and Grains Enriched breads. Cooked or ready-to-eat cereals. Tortillas,
dinner rolls, English muffins, melba toast, rusks, Zwieback,
saltines, crackers.
None
Fruits and vegeta-
bles
Non-citrus fruits and juices. All vegetables and their juices. Citrus, tomatoe, gas-forming vegeta-
bles (cabbage, cauliflower, etc)
Desserts Puddings, gelatins, sherbet, pound cake, cookies Any containing foods not allowed
Beverages Decaffeinated tea. Cereal beverages such as Postum. Juices as
allowed. Carbonated beverages as allowed.
Coffee, tea, decaffeinated coffee,
chocolate drinks, carbonated bever-
ages containing caffeine, alcoholic
beverages
The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
Sample Menu
Suggested Meal Plan Suggested Foods and beverages
Breakfast
Fruit Juice
Cereal with Milk
Meat/Meat Substitute
Bread/Margarine
Beverage
Apple Juice
Oatmeal with Milk
Soft Cooked Egg
Toast, Jelly
Milk, Decaffeinated Tea
Lunch
Soup
Meat/Meat Substitute
Vegetable
Fruit Juice
Dessert
Bread/Margarine
Beverage
Cream soup & crackers
Meat loaf without gravy
Buttered Green Beans
Apricot Juice
Lemon Sponge Pudding
Bread and Margarine
Milk
Supper
Juice
Meat/Meat Substitute
Vegetable
Dessert
Bread/Margarine
Beverage
Apple Juice
Sliced Baked chicken and noodles
Peas
Applesauce
Bread and margarine
Milk, decaffeinated tea
Nutrient Analysis
Calories 2 295 Kcal Vitamin A 1161 IU Calcium 1628 mg
Protein 111 gm Vitamin C 104 mg Phosphorus 2077 mg
Carbohydrate 266 gm Niacin 25 mg Zinc 12 mg
Fat 83 gm Riboflavin 2.9 mg Iron 12 mg
Cholesterol 573 mg Thiamin 1.9 mg Sodium 3939 mg
Dietary Fiber 13 gm Folate 281 mcg Potassium 3710 mg

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676● www.floridaamigos.com
LAPAROSCOPY
POSTOPERATIVE INSTRUCTIONS
Depending on your operation you may be discharged from the hospital several hours after your surgery is over, or in
1 or 2 days. To be discharged you must meet the following criteria:
1. Have adequate control of your pain with oral pain medicine
2. Tolerate any type of diet (liquids, soft, etc.)
3. Able to urinate on your own (in most instances)
4. Vital signs are stable (Blood pressure, temperature, pulse, respiration)
5. Feel as if you are capable of going home.
***YOU WILL NOT BE DISCHARGED UNLESS YOU MEET THESE CRITERIA
Things to expect:
1. You might bleed or spot for several days. Use only sanitary napkins, no tampons.
2. You might have pains in your shoulders, chest, and abdomen. This is caused from the gas used during the pro
cedure and is nothing to worry about. Lying flat might decrease the discomfort. Your pain control pre
scription should be used for these pains.
3. For seven days: rest, walk, drink plenty of fluids, take only showers, and don’t drive. Further activities will be
discussed at your 1 week postoperative visit.
4. For constipation: Drink 8-10 glasses of water, Surfak 2x daily, Milk of Magnesia 2 caplets or 30cc every-other-
day. You may take prunes each day and fiber (Citrucel)
5. You will have small band-aid-type dressings over your little incisions on your abdomen or a membrane glue
called Dermabond. If Dermabond is used do not rub oil-based lotions over incision until 10 days have
passed. The belly button incision should be cleaned with hydrogen peroxide by letting some drip into the
belly button and then showering. It is not necessary to clean it with your finger, a face cloth, or a Q-Tip.
Don’t worry if water or soap run over the incision. The incision can be dried by using a hair dryer at low
speed (cool setting) or by holding a reading lamp with a 40 watt bulb at a distance of about a foot for 5-10
minutes. Leave the belly button incision open to air/sun.
6. There are over-the-counter anti-scarring patches/creams available at most pharmacies. Just ask the pharma
cists if you would like to use them.
7. Wear loose clothing for 2 weeks as tight clothing will irritate the belly button and may cause infection.
8. Begin increasing your activity gradually at the instructions of your doctor and/or after seven days of initial heal
ing.
9. We generally recommend a bland diet for 7 days. Thereafter there are no restrictions.
10. Take your temperature at least twice a day for 4-5 days. If it should rise to 100.5 degrees or higher, please con
tact us at 305-596-3744. Someone will return your call and answer any questions.
11. Please keep your postoperative appointment. During that appointment we will review you surgery, determine
long-term plans and options, often look at pictures of your particular problem, review the pathology report,
and examine the operative site for healing evaluation.
For those who have had bladder repair surgery/incontinence surgery:
1. You may be discharged with a catheter attached to a leg bag.
2. You will be instructed on the care of this.
3. You will be brought into the office at a pre-determined time to have the catheter removed.
4. Once the catheter is removed, you must be able to urinate adequately or else the catheter may need to be
replaced.
5. On the average, after bladder repair surgery, it may take 1-2 weeks for the bladder to begin functioning
properly (due to swelling and edema)

The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
Notes and Questions
Here is a list of 10 common questions you should ask your doctor and his staff regarding your surgery and recovery.
1. What medications should I take and when? Take your pain medications as directed. Use all other medica-
tions you normally take.
2. What are the signs of infections and other common complications? Fever with redness and swelling at the
incision site; or worsening pain in the pelvic area. A urinary tract infection may produce pain with urina-
tion and frequency. A yeast infection usually has vaginal burning and discharge.
3. What should I eat? Bland diet for 7 days and then foods you choose to eat thereafter.
4. What will happen to my stitches/staples/Dermabond glue? The stitches are self-dissolving. Dermabond is
tissue glue that lasts 10 days. During this 10 days do not rub oils or lotions on this glue as it reduces its
strength. After 10 days you can rub oils on it and remove it. If staples are used (rarely) they will be re-
moved in the office at the 7 day postoperative visit.
5. When will I have my postoperative visit? 7 days after surgery and a possible 3 weeks after that.
6. When can I drive my car? Usually within 2 weeks and only after discontinuing narcotics.
7. When can I go back to work? This depends on your recovery and motivation
8. When can I shower/bathe? You can shower immediately, bath after 3 weeks
9. How much weight can I lift? Can I bend? You can bend as need and with caution. I generally recommend not
lifting more than a grocery bag during recovery.
10. When can I start sexual relations again? Sexual relations should start after full healing. This is usually 6-8
weeks, but may be as early as 4 weeks with laparoscopy
11. What are my calcium needs? All women need 1500 mgs calcium each day. This is divided between diet and
supplements.
12. When can I expect menopausal symptoms? You will only have these symptoms if your ovaries are removed.
They will begin 2-3 days after surgery and only if you do not start hormone replacement therapy.
13. Will I have a period after surgery? If you have had a hysterectomy you will not have a period. You may ex-
perience bleeding during the healing phase.

RECEIVING A BLOOD TRANSFUSION:
WHAT EVERY PATIENT SHOULD KNOW
How many Americans need blood each year?
Nearly five million Americans receive blood transfusions each year. Blood is used to save the lives of patients who need surgery or
other medical treatment, for trauma victims of accidents and burns and for patients with cancer, hemophilia, and other serious
diseases.
Why would my doctor recommend that I receive blood?
You may need to receive blood in order to stabilize a medical condition or to save your life. The amount of blood that is given to
you is a decision your physician will make based on your particular needs. Details about why you may need blood will be best
explained by your doctor.
What steps are taken to make sure that the blood patients receive is safe?
There are many safeguards on our national blood supply to ensure safe blood for patients. First, blood is donated by volunteer
donors. Before giving blood, donors must answer questions about their health and risk factors for disease, and only a person with
a clean bill of health can give blood. Blood from each accepted donor goes through extensive testing. In addition to tests for blood
type, nine separate screening tests are run for evidence of infection with hepatitis, HIV, HTLV and syphilis. Finally, a carefully iden-
tified blood sample is tested against blood from the patient who will receive it, a process called crossmatch.
What are the risks of receiving blood?
If a blood transfusion is indicated during a surgical procedure or other medical treatment, the risks of NOT receiving blood far out-
weigh the risks of transfusion. Some patients may experience minor changes in the body's immune system after a transfusion,
causing mild symptoms, such as fever, chills or hives, which typically require little or no treatment. A small number of patients may
also react to donated blood by developing antibodies (immune reactions).
The transmission of disease and the destruction of red blood cells occur only very rarely, and seldom threaten life. The potential
risk of contracting AIDS from a blood transfusion has received a great deal of attention. But it is important to know that all donated
blood in the United States is tested for the AIDS virus, reducing the risk to a negligible level. When you consider the risks of trans-
fusion, it may be helpful to know that many common activities carry far greater risks — for example, smoking cigarettes, driving a
car or being pregnant.
What can I do to make sure that a safe supply of blood will be available should I, my friends, family or members of my
community need it?
It is very important that healthy Americans donate blood. This will guarantee that a safe and adequate blood supply is available for
patient care. Millions of lives are saved each year because of the availability of donated blood.
Do I have choices other than receiving blood from the community blood supply?
Yes, you may have other choices. Autologous blood transfusion refers to procedures in which you may serve as your own blood
donor. In preoperative autologous donation, your blood may be collected and stored before a scheduled surgery if blood use may
be required. In intraoperative and postoperative autologous transfusions, blood lost during surgery is saved and returned to the
patient. Directed donations can also be arranged in some cases from a person (usually a friend or relative) whom you select.
BLOOD TRANSFUSIONS
Why is blood transfused? Transfusions are given to replace blood lost during surgery, to replace blood lost because of acci-
dents, and to replace blood lost due to internal bleeding caused by a condition such as stomach ulcers. Transfusions are used in
the treatment of cancers such as leukemia and to treat different types of anemia such as sickle cell disease and thalassemia.
Is there a charge for receiving blood?
All blood centers and hospitals charge a processing fee to cover service costs such as donor recruitment; collecting, testing, pack-
aging, storing and distributing the blood; and administrative and staff costs. In the hospital, there are charges for matching and
administering a blood transfusion. Most health insurance policies cover these fees.
Are there any risks in receiving a transfusion?
As with any medical procedure, blood transfusions carry some risk. There is a remote chance of receiving blood of the wrong type.
In addition, several infectious diseases can be transmitted by blood transfusions. Among the viruses that may be transmitted by
blood are: human immunodeficiency virus (HIV), the virus that causes AIDS; human T-cell lymphotropic virus (HTLV-I); several
hepatitis viruses; cytomegalovirus (CMV), and West Nile virus (WNV). However, the very small risk of acquiring such a virus is
outweighed by the benefits of a blood transfusion that is needed.
What steps are taken to reduce the risks involved in receiving a transfusion?
Steps to ensure maximum transfusion safety involve both donor and recipient. Donors are screened very carefully using a detailed
questionnaire for health problems or circumstances that increase risk of transmitting infection. After blood has been drawn, it is
tested for numerous viruses and other potentially harmful disease agents, and positive or doubtful units are discarded. Donor
blood is tested for ABO, Rh and the presence of possibly dangerous blood group antibodies. After the recipient's blood has been
tested for ABO, Rh and the presence of blood group antibodies, donor units are selected that lack antigens that might react with
any antibodies present in the recipient. Additional checks are then performed to compare the specific donor unit selected with the
patient's blood.
What steps are taken to reduce the risk of acquiring hepatitis from transfusions?
First of all, donors are questioned extensively about possible exposure to hepatitis and behaviors that put them at increased risk
for hepatitis. Individuals who are found to have had an exposure or a risk factor are deferred from donation. In addition, several
tests are used to detect the presence of hepatitis B and C. Since the 1970s, all donor blood has been tested for direct evidence of
the hepatitis B virus. Since 1986, all donated blood has been screened for indirect evidence of hepatitis B, using a test for one of
the antibodies to hepatitis B (antibody to hepatitis B core antigen). A test for antibody to hepatitis C virus is also in place. Hepatitis
A is very rarely transmitted through blood transfusion.
What is cytomegalovirus (CMV)?
CMV is a common virus that causes a mild to unnoticeable infection in healthy people. About half of the adult population in the
United States has been infected with CMV. The virus can be transmitted by blood transfusion. Although it is not a problem for most
The Association of Minimally Invasive
Gynecologic Surgeons
…dedicated to healthy lifestyles and safe, state-of-the-art, innovative surgery for women of all ages
8740 N. Kendall Drive, Suite 101, Miami, Florida 33176
Phone 305 596 3744 ● fax 305 596 3676 ● www.floridaamigos.com
transfusion recipients, it can cause serious disease in patients whose immune systems function poorly, such as premature infants
and patients who have undergone tissue or organ transplantation. These patients frequently are given blood that has been
screened or processed in such a way as to reduce the risk of CMV transmission.
What is human T-cell lymphotropic virus?
Human T-cell lymphotropic virus, type I (or HTLV-I) is considered a leukemia virus; it differs from the virus that causes AIDS (HIV).
HTLV-I is found particularly in Japanese people and in people living in the Caribbean area. HTLV-I can, on occasion, cause leuke-
mia and a paralytic disease of the nervous system, but it takes many years to do so.
Are tests done to detect venereal disease?
Yes. Blood is tested for evidence of syphilis infection.
What other donor screening for infectious diseases is done?
Donors who are at risk of transmitting malaria are screened by medical history and rejected as blood donors. As a result, very few
recipients of blood transfusions in the United States develop malaria. Similarly, individuals known to be harboring other infectious
diseases are deferred or rejected as blood donors.
How have tests performed on donated blood affected the supply?
Blood and components are tested to eliminate units that may carry HTLV-I, -II, HIV, hepatitis B and hepatitis C, as well as those
that are positive for syphilis. Approximately 1.7 percent of whole blood units are discarded due to positive tests. False positives
may occur due to the sensitivity of the testing procedure. This means that some units of blood are discarded, although the donor
does not have a viral infection. It is very important that units that are true positives not be used for transfusion. Until more research
is done to perfect testing procedures that will detect only true positives, blood banks and donor centers will continue to take pre-
cautions to ensure the safest blood supply possible; this will include not using blood with a false-positive test result.
Has there been any progress in developing blood substitutes?
Blood substitutes with the ability to carry oxygen have been used in animals and to a limited extent in humans. Most blood substi-
tutes have not been proven totally safe or completely effective. These substitutes do not provide clotting factors or white cells to
fight infection. Most blood substitutes under development remain highly experimental, and none has been licensed for use in the
United States. Research into substitutes is continuing, however.
BLOOD SAFETY ISSUES
The American Association of Blood Banks (AABB), through its nearly 2,000 institutional and about 8,000 individual members, is
committed to ensuring a safe and adequate blood supply for the American people. AABB continually takes steps to enhance safety
by evaluating new technology as it becomes available. AABB assesses and, when the specific technology is deemed effective and
feasible, promotes implementation of new technology at the blood bank level through its Standards for Blood Banks and Transfu-
sion Services. As a result of AABB's development of a multi-layer safety system, which includes donor screening, donor deferral,
and testing, transmission of transfusion-transmitted diseases has diminished steadily over the years.
Standards
The AABB has systems in place that ensure continual review and refinement of its voluntary standards. A standing committee is
assigned to review and update the entire publication of AABB Standards for Blood Banks and Transfusion Services every 18
months. Interim standards may be issued to reflect new technologies, methods, or criteria for donor selection if it is determined,
based upon available data, that they will enhance the safety of the blood supply during the intervening periods.
Systems for ensuring the safety of the blood supply generally are described as having five layers, which work together to screen
out infectious agents. Every blood collection center follows essentially the same requirements, all of which are specifically set forth
in the AABB Standards. AABB standards (for which compliance is required of members) are based upon established best prac-
tices and in accordance with FDA regulations and guidelines.
Layer 1: Blood Donor Screening
Efforts are made to recruit volunteer blood donors only from the safest and most suitable donors. For example, blood is collected
from universities and workplaces, but not from prisons. Blood for transfusion is collected from volunteer blood donors. Improper
donor incentives and coercion, which could alter the truthfulness of some donors, are prohibited.
Layer 2: Individual Screening
Each individual blood donor is required to read information about blood safety and is encouraged to leave, without explanation, if
he or she recognizes that giving blood would be inappropriate. Potential donors are also asked a series of questions about their
health and lifestyle (including direct questions on sexual behavior designed to identify high-risk activities) and undergo a miniphysi-
cal before being allowed to donate. The questions and examinations are designed to prevent individuals who are at high risk for
HIV, hepatitis and other infectious diseases from donating blood. This process is continually refined in order to ensure that blood is
drawn from the most appropriate individuals.
Layer 3: Laboratory Testing
The third layer involves testing collected blood for possible infectious diseases. Nine laboratory tests for different infectious dis-
eases are currently conducted on each unit of donated blood. All results must be negative for a blood unit to be labeled and re-
leased. Tests for hepatitis B and syphilis were in place before 1985. Since 1985, the following tests have been implemented: HIV-1
and -2, HIV antigen, HTLV-1 and -2, two tests for hepatitis B and a test for hepatitis C. Nucleic acid amplification testing (NAT)
employs a form of testing technology that directly detects the genetic material of viruses like hepatitis C and HIV. An investiga-
tional NAT to screen for West Nile virus is now available.
Layer 4: Confidential Exclusion
Blood donors may be offered a confidential opportunity to exclude their blood from use in transfusion by attaching stickers to the
paperwork identifying the collected unit for use or withdrawal. If a donor knows of any reason why his or her blood should not be
used for transfusion, he or she places the sticker indicating that the unit should not be transfused on the label. This is done
to
ensure that no pressure is exerted on the donor to give blood.
Layer 5: Donor Record Checks
Every donation is checked against existing records. If a donor has been indefinitely deferred, the collected unit is withdrawn from
circulation and potential use. This process acts as a barrier to prevent the release of any blood from a donor who was previously
judged to be indefinitely unacceptable